While CPAP (Continuous Positive Airway Pressure) machines are the gold standard for treating sleep apnea, they aren’t a one-size-fits-all solution. Many individuals start using CPAP to address their sleep apnea but find themselves unable to continue for various reasons.
Some key reasons why people might seek alternatives to CPAP are the mask feeling bulky and claustrophobic, the disruptive noise of the machine, and frustrating leaks around the mask. Also, CPAP therapy can dry out the nose and throat, causing discomfort.
This guide explores various alternatives to CPAP machines, emphasizing the importance of personalized treatment approaches for effective sleep apnea management.
Oral Appliances: A Comfortable Substitute
Oral appliances serve as a primary non-CPAP solution for sleep apnea, offering comfort and effectiveness. These appliances come in various types, each designed to address specific needs and severity levels of sleep apnea. By gently repositioning the jaw or tongue, these devices help keep the airway open during sleep, reducing the risk of obstructive sleep apnea episodes.

From mandibular advancement devices to tongue-retaining devices, there’s a range of options available to suit different individuals and preferences. They are generally most effective for mild to moderate sleep apnea, but their suitability can vary depending on individual anatomy and doctor’s assessment.
Mandibular Advancement Devices (MADs)
Mandibular Advancement Devices (MADs) are custom-made mouthpieces resembling retainers, worn during sleep. They gently push the lower jaw forward, increasing the space behind the tongue and preventing its collapse, which can obstruct the airway and cause sleep apnea.
A dentist creates a custom MAD after taking precise measurements of your mouth and bite. Regular follow-up appointments may be necessary to adjust the device for optimal comfort and effectiveness.
Several studies including this research paper show MADs are most effective for mild to moderate sleep apnea. They can significantly reduce sleep apnea events, improve sleep quality, and decrease daytime sleepiness. However, they may not be suitable for everyone, particularly individuals with severe obstructive sleep apnea, jaw problems, or claustrophobia.
Important to Note: Consulting a doctor or dentist to determine if MADs are an appropriate treatment option for your specific sleep apnea case is crucial.
Tongue Retaining Devices (TRDs)
Unlike MADs that focus on the jaw, TRDs are oral appliances designed to address the tongue’s role in sleep apnea. These mouthpiece-like devices hold the tongue in a forward position throughout sleep, aiming to prevent the tongue from collapsing backward and blocking the airway.
They maintain the correct tongue resting position, promoting unobstructed breathing.
TRDs offer a non-invasive alternative to traditional CPAP machines for sleep apnea, potentially improving comfort and adherence. Compared to MADs, TRDs may cause fewer jaw-related side effects like discomfort or pain. However, these oral appliances can contribute to dry mouth or drooling due to altered airflow patterns during sleep and tongue position.
The appliance itself might cause some initial irritation to the tongue. While TRDs show potential in mild sleep apnea cases, they are generally less effective than MADs for treating sleep apnea.
Positional Therapy: Targeting Sleep Posture
Sleep apnea severity can be significantly influenced by sleep position. Sleeping on your back is often associated with worsened symptoms due to gravity pulling your tongue and soft tissues back, narrowing the airway. Conversely, sleeping on your side (lateral) can help keep the airway open and reduce sleep apnea events.
Positional therapy leverages this knowledge to encourage side sleeping and alleviate sleep apnea symptoms. Using devices like wedge pillows, back packs, or tennis balls placed behind your back can act as gentle reminders or physical barriers to prevent rolling onto your back.
To maintain side sleeping, full-body pillows or specially designed sleep shirts can provide gentle support and promote staying on your side throughout the night.
While not a cure, positional therapy can significantly reduce sleep apnea events and improve sleep quality for some individuals, especially those with mild to moderate sleep apnea. It offers a non-invasive and readily accessible approach compared to other treatment options.
Lifestyle and Behavioral Changes
Beyond medical interventions, several lifestyle adjustments can significantly impact sleep apnea severity.
- Losing even a small amount of weight can reduce excess tissue in the upper airway, allowing for easier breathing during sleep.
- Additionally, avoiding heavy meals and maintaining a healthy diet can improve sleep quality and potentially reduce pressure on the airway.
- Limiting alcohol intake, especially before sleep, helps maintain muscle tone in the upper airway, and reduces the risk of airway collapse.
By incorporating these changes alongside your doctor-recommended treatment plan, you can actively contribute to managing your sleep apnea and improving your overall sleep quality. Let’s delve deeper into how to adjust to these lifestyle changes.
Weight Loss and Exercise
Obesity is a major risk factor for sleep apnea. Excess weight contributes to fatty tissue deposits around the neck and upper airway, narrowing the passage for air and increasing the risk of collapse during sleep.
Weight loss, even a modest amount, can significantly improve sleep apnea symptoms. By reducing the amount of tissue narrowing the airway, breathing becomes easier and the frequency of apneic events decreases. Additionally, regular exercise strengthens muscles that support the airway, further helping to keep it open during sleep.
Therefore, weight management and exercise become crucial allies in managing sleep apnea alongside other treatment options prescribed by your doctor. Their combined impact can significantly improve sleep quality and overall health.
Dietary Adjustments and Alcohol Reduction
Dietary choices and alcohol consumption can significantly influence sleep apnea severity. Large, heavy meals close to bedtime can relax throat muscles, increasing the risk of airway collapse and sleep apnea episodes. Also, certain foods like fried foods and processed meats can contribute to inflammation, potentially worsening sleep apnea symptoms.
Alcohol can also disrupt sleep patterns and fragment sleep, leading to more frequent awakenings and potentially worsening sleep apnea. It acts as a muscle relaxant, further weakening the muscles that support the airway and increasing the risk of collapse during sleep.
Maintaining a healthy diet by limiting heavy meals and inflammatory foods before bed, and minimizing alcohol intake, can be crucial steps in managing sleep apnea and improving overall sleep quality.
Innovative Devices and Airway Technologies
Several alternative technologies and approaches are available to use instead of CPAP, each with diverse mechanisms, usability, and effectiveness. Nasal strips, dilators, and mouth tapes are non invasive alternatives, elevating nasal breathing.
Minimally invasive implants such as Hypoglossal Nerve Stimulation (HGNS) and Expiratory Muscle Stimulation (EMS) can also reduce sleep apnea.
Nasal Strips and Dilators

Snoring and sleep apnea can be exacerbated by congested nasal passages, which force individuals to breathe through their mouth. Nasal strips and dilators offer a non-invasive and readily available solution to promote nasal breathing and potentially improve sleep quality.
Nasal strips are adhesive patches applied across the bridge of the nose. They gently lift and support the sides of the nostrils, creating more space for airflow. Explore our overview of the best nasal strips for snoring to pick the suitable one as a CPAP alternative.
Nasal dilators come in various forms, including spring-like inserts or soft, expandable devices placed inside the nostrils. They work by gently widening the nasal passages from within.
By opening up the nasal passages, nasal strips, and dilators can facilitate easier breathing during sleep. They also reduce the vibrations in the airway that cause snoring. These devices can offer mild relief from nasal congestion caused by allergies or colds.
Mouth Tape & CPAP

Mouth taping is simply applying a strip of hypoallergenic tape over the lips during sleep to encourage nasal breathing. While gaining popularity for improved sleep, its use in treating sleep apnea remains controversial and requires careful consideration.
If we talk about the potential benefits, mouth taping can encourage individuals who primarily breathe through their mouth to switch to nasal breathing during sleep. As a result, there is less vibration in the airway, which curbs snoring. Read our top rated mouth tapes guide for safe and recommended options.
On the flip side, the effectiveness and safety of mouth taping for sleep apnea lack extensive scientific evidence. It might cause dry mouth, claustrophobia, and difficulty breathing in some individuals. Mouth taping should not be considered a substitute for CPAP therapy in individuals diagnosed with moderate or severe sleep apnea.
Sleep specialists generally advise against using mouth taping for sleep apnea due to the lack of conclusive evidence and potential risks.
The combination of mouth taping and CPAP therapy might work well for some patients. However, using them in combination for sleep apnea warrants significant caution.
Firstly, there is limited evidence to suggest that using mouth tape alongside CPAP therapy significantly improves sleep apnea outcomes. Mouth taping could interfere with the CPAP mask seal, compromising its effectiveness in delivering positive airway pressure.
Combining mouth dryness from taping with the inherent dryness associated with CPAP machine use can significantly worsen sleep comfort and adherence to therapy. In certain scenarios, mouth taping might lead to rebreathing of exhaled air, potentially impacting CPAP efficacy and increasing CO2 levels.
If you suffer from mild sleep apnea and do not want to opt for CPAP therapy, a safe option could be Hostage Tape, which is a comfortable yet strong grip that helps elevate nasal breathing.
Advanced Surgical Interventions for Obstructive Sleep Apnea (OSA)
While not a first-line approach, advanced surgeries can be options for severe or treatment-resistant sleep apnea after consultation with a healthcare professional and careful consideration of risks and benefits. These procedures aim to physically widen the airway and improve breathing during sleep.
- Maxillomandibular advancement (MMA): This surgery surgically advances the upper and lower jaw, creating more space for the tongue and soft tissues in the airway.
- Hypoglossal nerve stimulation (HGNS): A minimally invasive implant gently stimulates the tongue muscle, keeping the airway open during sleep.
- Genioglossus advancement: Surgically advances the chin bone to increase space behind the tongue.
- Nasal surgery: Corrects structural abnormalities in the nose that impede airflow.
- Adenoidectomy: Removal of enlarged adenoids to improve nasal breathing.
- Uvulopalatopharyngoplasty (UPPP): Removes excess tissue in the soft palate and throat to widen the airway.
- Tongue reduction surgeries: Various procedures to reduce tongue volume for severe sleep apnea, typically used as a last resort due to potential complications.
Supportive Accessories & CPAP Machine
While CPAP therapy remains a cornerstone of treating sleep apnea, various supportive accessories can enhance comfort and adherence. Ergonomic pillows, custom mouthpieces, chinstraps, and humidifiers can effectively help in managing sleep apnea.
Exploring the potential benefits and suitability of these accessories for your specific case with a healthcare professional is crucial.
Memory Foam Ergonomic Pillow
For individuals with sleep apnea, choosing the right pillow can significantly improve sleep quality and treatment effectiveness. Our selected Derila pillow is one of the best pillow for CPAP users. Derila is the memory foam ergonomic pillow, designed specifically to maintain a neutral spinal alignment, and allow comfortable side sleeping position.
Ergonomic pillows made with memory foam address sleep apnea by providing proper head and neck support, reducing pressure on the airway, and preventing collapse during sleep. Some ergonomic pillows feature curved or cut-out sections designed to cradle the head and neck comfortably in side sleeping positions, which is generally recommended for individuals with sleep apnea.
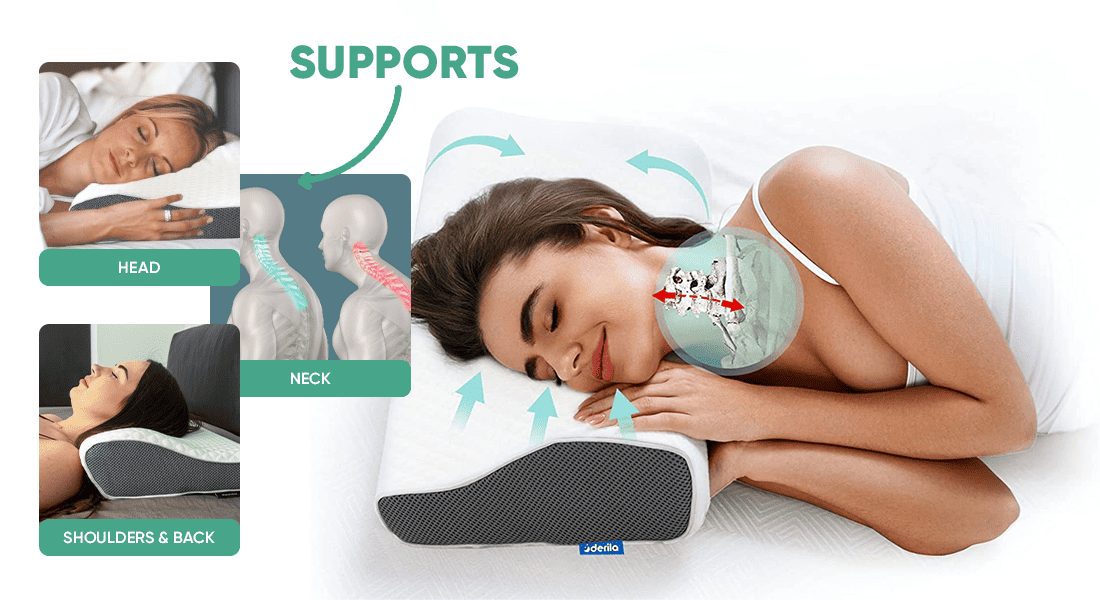
If using an ergonomic pillow sounds like the ultimate solution to support your sleep apnea management, Derila pillow is probably the best option you could have. By supporting proper neck alignment, the Derila pillow can help prevent the tongue and soft tissues from collapsing and obstructing the airway.
Custom-Fitted Mouthpieces
Custom-fitted mouthpieces, also known as oral appliance therapy (OAT), is a type of medical device used to treat mild to moderate sleep apnea. Unlike over-the-counter mouthpieces, which are one-size-fits-all, custom-fitted oral appliance options are created based on precise measurements of your mouth and jaw structure.
Individually designed to ensure a comfortable and effective fit, the custom mouthpiece potentially leads to better treatment outcomes and improved sleep quality compared to generic mouthpieces.

Custom mouthpieces, also known as mandibular advancement devices (MADs), are tailored to an individual’s mouth. They work by slightly advancing the lower jaw forward during sleep, which helps keep the airway open and reduces snoring.
While MADs are primarily designed to address snoring, they can also be effective in treating mild to moderate obstructive sleep apnea (OSA). Premium quality MADs such as the VitalSleep mouthpiece can reduce the frequency and severity of apnea events in some individuals. However, their effectiveness may vary depending on factors such as the severity of OSA and individual characteristics of the patient’s anatomy.
Consulting with a healthcare professional helps determine the suitability and effectiveness of custom mouthpieces for treating sleep apnea.
Emerging Research on CPAP Alternatives
Emerging research in sleep apnea treatment suggests a shift towards a more individualized approach, moving away from the traditional “one treatment fits all” model.
According to a 2022 study, proper patient selection and the use of specific criteria for non-CPAP treatment are vital for optimal outcomes. The same study establishes that mandibular advancement devices are currently the most commonly used non-CPAP treatment.
Ongoing studies explore innovative therapies, such as neuromodulation and biocompatible implants, aiming to provide effective alternatives for patients unable to tolerate or benefit from CPAP therapy. Additionally, established options like hypoglossal nerve stimulation are further being researched to optimize their effectiveness and accessibility.
Personalizing Your Sleep Apnea Treatment
While CPAP machine therapy remains a mainstay in treating sleep apnea, numerous CPAP alternatives offer potential benefits. Weight management, dietary adjustments, and avoiding alcohol can significantly improve symptoms. Custom-fitted mouthpieces aid in airway openness in mild to moderate cases.
Advanced therapies like minimally invasive implants or nerve stimulation techniques are emerging CPAP alternatives for specific cases. However, one-size-fits-all solutions rarely exist. Consulting and collaborating with healthcare professionals is vital to accurately diagnose sleep apnea and determine its severity, and pick options based on individual needs.
By working together, you and your healthcare team can navigate the path toward a personalized and effective sleep apnea treatment strategy.